Watching Brief
| Title | Legionnaires’ disease: A critical report of the pneumonia of unknown origin outbreak in Argentina |
| Authors | Evangeline Reiko Kenrick Gardiner, Adriana Notaras, Mohana Priya Kunasekaran, Ashley Quigley |
| Date of first report of the outbreak | 18 August 2022 [1]. |
| Disease or outbreak | Pneumonia due to unknown cause (suspected Legionnaires’ disease). |
| Origin (country, city, region) | Argentina |
| Suspected Source (specify food source, zoonotic or human origin or other) | |
| Date of outbreak beginning | 18 August 2022 [1]. |
| Date outbreak declared over | Although no new cases have been reported since 8 September 2022 [3], the outbreak has not officially been declared over. |
| Affected countries & regions | San Miguel de Tucumán, Argentina. |
| Number of cases (specify at what date if ongoing) | 22 suspected cases (six deceased) as of 8 September 2022 (four results compatible with Legionella pneumophila and one with Legionella spp.) [3]. |
| Clinical features | The initial 11 identified cases presented with [1]:
|
| Mode of transmission (dominant mode and other documented modes) | Legionnaires’ disease occurs via inhalation of aerolised water containing the Legionella bacteria which is present in numerous freshwater areas [4]. The bacteria are usually at undetectable levels which do not lead to infection or disease [4]. Still water, increased temperatures or the presence of debris or biofilm can cause the bacteria to proliferate, becoming more detectable and infectious [4]. Therefore, frequent sources of infection include potable water, cooling towers, spas and fountains [5]. In recent years in the United States (US), drinking water has become a more common source of infection compared to cooling towers [6]. One occurrence of potential human-to-human transmission of Legionella has been recorded, between a mother and son in Portugal [7]. The son (who worked at a cooling tower) developed severe respiratory symptoms including a cough with his mother developing symptoms nine days later. As Legionella pneumophila was only found in the cooling tower and not in the home of either the mother or son, it is probable that human-to-human transmission occurred [7]. |
| Demographics of cases | As of 8th September, a total of 22 cases have been reported [3,8]. There are a total of eight healthcare workers, nine patients and five family members or carers infected [8]. Currently, four of the cases are receiving treatment in hospital [8]. The most updated demographic details were released on 5 September for only 11 cases in the outbreak. The median age of these 11 cases is 45 years, with the youngest case being 30 years old and the oldest being 81 years old [1]. Seven were male and most cases had prior conditions and/or risk factors for serious illness, including four who passed away [1]. Three of those who passed away were healthcare workers who had direct contact with infected patients. |
| Case fatality rate | The case fatality rate (CFR) for Legionnaires’ disease may be as high as 40-80% in untreated immunocompromised individuals, reducing to between 5-30% if they receive appropriate case management and treatment [5]. Overall, the CFR is generally between 5-15%, increasing up to 30% for nosocomial infections [5,9]. The CFR for this current outbreak in Argentina is 27.3%.
|
| Complications | The most frequently reported complication of Legionnaires’ disease is severe pneumonia, which can become fatal [5]. Approximately one-third of these patients will develop hemoptysis [5]. Severe pneumonia often leads to shock and/or multi-organ failure, particularly of the lungs and kidneys [5]. Untreated disease often becomes more severe in the first seven days, with pneumonia progressing and increasing the risk of brain sequalae and death [5]. Research has shown that pneumonia patients admitted to intensive care with severe illness more frequently re-present to hospital and experience adverse health outcomes, such as chronic and acute kidney disorders, in the five years following initial diagnosis [10].
|
| Available prevention | There are no vaccines available to prevent Legionnaires’ disease [11]. Prevention methods focus on water management across different community and workplace settings, with a particular focus on human-made water systems including cooling towers, spas, showerheads and sinks, hot water tanks and large plumbing systems [11]. Once risk areas for Legionella growth are identified, they should be targeted with control measures including elevated temperatures and added disinfectant [12]. This should be followed by routine monitoring including the checking of temperatures, disinfectant levels, water quality and visual inspections for debris and visible biofilm [12]. Environmental assessments and regular environmental sampling are also recommended. In collaboration with an infection control specialist, health care settings must have effective water management programs instituted to reduce the risk of nosocomial Legionnaires’ disease [13]. Common control methods used across hospital settings include water chlorination, increasing heat temperature, implementing bacteriological barriers with a filter, and the addition of silver and copper ions to water [13].
|
| Available treatment | Treatment for Legionnaires’ disease follows the treatment guidelines for community-acquired pneumonia where amoxicillin, doxycycline or macrolide is given to patients in the community with no comorbidities or risk factors for Methicillin-resistant Staphylococcus aureus (MRSA) or Pseudomonas aeruginosa [14]. For those with comorbidities in the community, combination therapy with amoxicillin/clavulanate or cephalosporin and macrolide or doxycycline or monotherapy with respiratory fluoroquinolones given. For hospital admitted patients, with mild to moderate pneumonia, B-lactam plus macrolide or respiratory flurioquinolone is given whilst patients with severe pneumonia are treated with B-lactam plus macrolide or B-lactam plus fluriquinolone. Continued routine monitoring of patients post diagnosis, with appropriate medical intervention including non-mechanical or mechanical ventilation and chest X-rays dependent on the patients’ clinical status and to justify additional treatment or management is suggested [14]. |
| Comparison with past outbreaks | There have been 168 reported Legionnaires' disease outbreaks across 24 countries, with a total of 6,968 cases and 365 deaths [15]. Most of the outbreaks have occurred in the community (47%), but also in locations such as hospitals (14%), hotels (9%) and assisted living facilities (6%) [15]. Of 19 Legionnaires’ disease outbreaks in Europe in 2020, 47% were associated with hospital settings compared to less than 28% of outbreaks from 2016 to 2019 linked to hospital settings [16]. The largest of these outbreaks was in Portugal, with a total of 88 confirmed cases reported between October and November 2020 [17]. The source was presumed to be a common outdoor airborne exposure located between Matosinhos and Vila de Conde [17]. Suspected sources were investigated in areas with the highest numbers of cases, resulting in the closure of cooling towers that tested positive for Legionella spp. and Legionella pneumophila [17]. The outbreak response faced many challenges as this was the first Legionnaires’ disease outbreak during the COVID-19 pandemic in Portugal. The health system was already overburdened, and overlapping clinical presentations of COVID-19 and Legionnaires’ disease may have led to delayed diagnoses of cases [17]. In the current outbreak, health authorities in the Tucumán Province are collecting clinical and environmental samples to define the source of contamination [1]. This outbreak response may be facing similar challenges to the 2020 outbreak in Portugal, as ongoing COVID-19 cases remain a burden to health systems, and overlapping clinical presentations of COVID-19 and Legionnaires’ disease may lead to misdiagnosis. |
| Unusual features | There are emerging reports suggesting that the pneumonia outbreak in Argentina is not an outbreak of Legionnaires’ disease, with staff from the affected hospital protesting these claims and the closure of the facility [18,19]. According to local physicians, patients are presenting with gastrointestinal symptoms together with pneumonia, which are not typical of Legionnaires’ disease [20]. Additionally, there are reports of similar outbreaks emerging in a hospital in Mendoza (approximately 960km away from Tucumán) and in a college in Tucumán where 60 cases of gastroenteritis have been reported in students [20,21]. This has caused some local health professionals to question the validity of labelling this an outbreak of Legionnaires’ disease, as cases should not be appearing in different locations and official confirmation by the Ministry of Health of Tucumán has not yet been provided. |
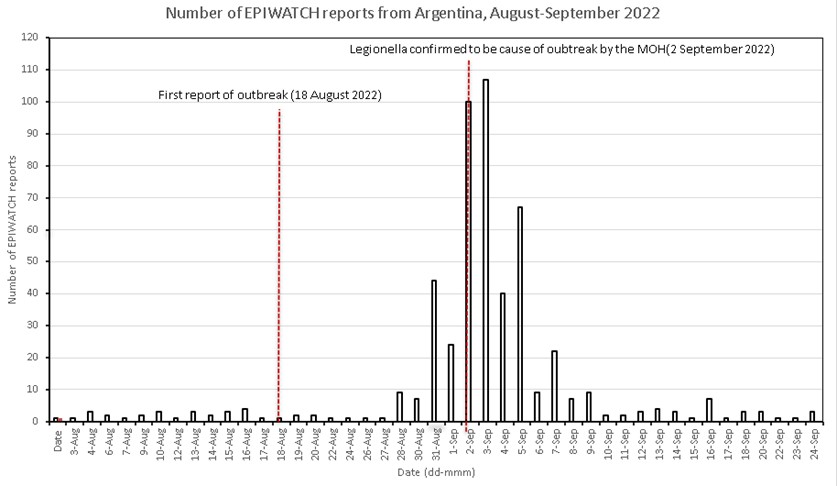
| Critical analysis | Initial laboratory testing has isolated Legionella pneumophila and Legionella spp. as the causative agent of this pneumonia cluster, ruling out COVID-19, hantavirus and influenza [22]. However, health professionals in Argentina have voiced allegations that Legionella may not be the cause of this outbreak [18,19,20]. More information is needed regarding the current outbreak to address the controversy. Figure 1 displays the number of EPIWATCH reports in Argentina during the time of the outbreak. Each report refers to a news article that has been collected by EPIWATCH, an open-source epidemic intelligence system [23]. There was an increase of reports in Argentina from the 28 August 2022, ten days from the first report on 18 August 2022. The peak of the reports was a day after the Ministry of Health in Tucumán reported Legionella pneumophila as the cause of the outbreak, with the number of reports decreasing since then. Further confirmation of these early results is needed through identification of the bacteria in environmental samples, matching of environmental samples to patient samples and wider testing of those affected by the outbreak.
Figure 1
Number of EPIWATCH reports from Argentina, August-September 2022. Official confirmation of Legionnaires’ disease outbreaks are complex. The availability of a clinical strain for comparison with an environmental strain is crucial in outbreak investigations to identify a source and pattern of spread [24,25]. The diagnosis of Legionnaires' disease is based on the combination of the presence of clinical symptoms, laboratory tests and environmental sample isolation [26]. However, these tests are not routinely performed by most clinical microbiology laboratories [26]. Using these methods to identify Legionnella as the source of an outbreak faces many challenges including diagnosis speed (results could take up to 2 weeks), reduced sensitivity and inadequate clinical samples (for example, insufficient sputum) [27]. According to a 2019 study, 4.4% of the community acquired pneumonia cases were caused by Legionella pneumophila in Córdoba [28]. However, most of these cases were diagnosed by urinary antigen detection which is a technique of rapid diagnosis with about 70% sensitivity, used for patients who are not able to produce enough sputum for culture [29]. Overall, the incidence of Legionella pneumophila infection in the country is low and is considered a rare cause (2%) of community acquired pneumonia in Argentina [30,31]. Potential misclassification of this outbreak may result in an over-emphasis of response activities and measures specific to Legionnaires’ disease. Additionally, the restrictive definition of cases to the single health facility in the absence of an identified source may result in missed cases. |
| Key questions | Confirmation of a Legionnaires outbreak is complex and matching of patient samples with environmental source samples is needed to confirm an outbreak of Legionnaires’ disease. Has this been confirmed by the Ministry of Health in Tucumán? Are all potential cases being tested or is the current case definition restrictive? What are the implications of potential human-to-human transmission of Legionnaires’ disease in the current and future outbreaks? What is the cause of increased outbreaks of Legionnaires’ disease in hospital settings across Europe since 2020? Could a vaccine be developed to prevent Legionnaires’ disease? |